Capstone Engineering Project
Building a Transabdominal Pulse Oximeter for Improved Fetal Monitoring
My Impact & Learned Skills
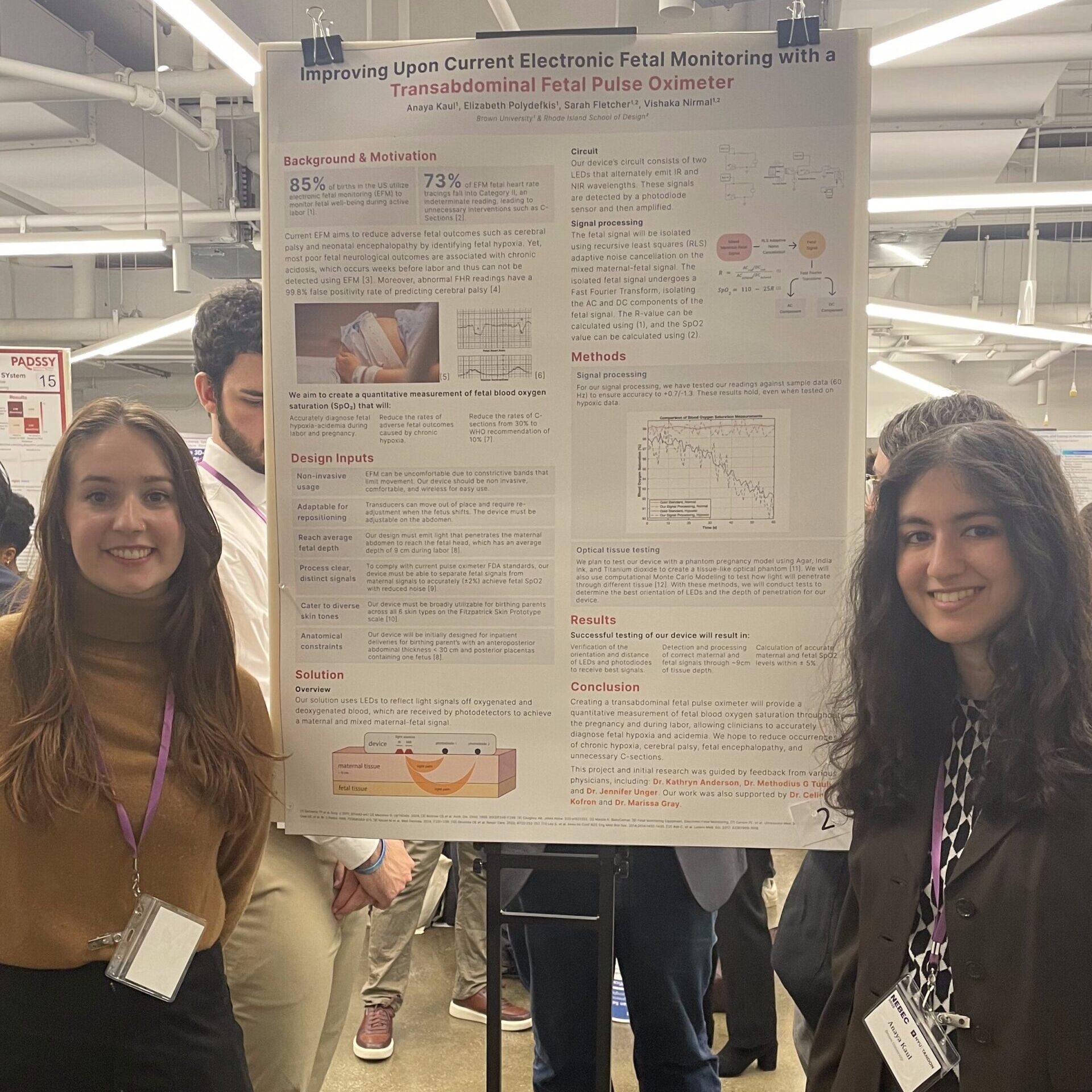
Presenting my Work at NEBEC at NYU
Throughout this project, I led the team’s circuitry design and performed a significant amount of the research into pulse oximetry technology to investigate how we could mirror current systems in our innovative device. I optimized our device throughout the prototyping process and put previously learned skills from the classroom in circuits and optics into actual practice to create our functioning device. I created a plan for how our device would be integrated in the medical system by doing research into current reimbursement structures and concluded that our device would work in tandem with current EFM to be easily integrated into current birth packages paid by insurers. I consulted with shareholders, from professors, to OB/GYNs, to entrepreneurs to understand how our device could satisfy various needs. Throughout the project, I practiced public speaking and how to effectively communicate technical information to various audiences. My work was selected for the Northeast Bioengineering Conference (NEBEC) at NYU and I presented it to a large audience. This project gave me ample experience and knowledge to understand how device design occurs along its pipeline from start to finish in industry and has grown my passion for developing innovative healthcare technologies.
99.8% of pregnancies
are found to be falsely positive for predicting cerebral palsy using current electronic fetal monitoring
85% of births
are performed using electronic fetal monitoring, which utilizes fetal heart rate to diagnose if interventions are needed
30% of births
are via C-sections due to EFM’s overpredictive nature for complications, much higher than the WHO’s recommended rate of 10% of births
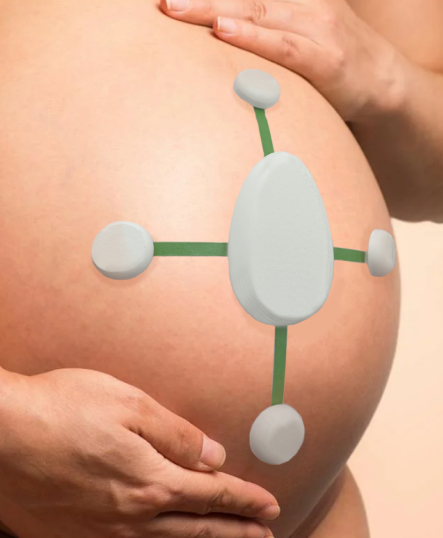
Prototype of Product Casing with Pregnancy
As part of my Engineering Capstone, my group and I designed a non-invasive Transabdominal Pulse Oximeter for sensing oxygen saturation levels in a fetus during labor. We sought to create an alternative monitoring system to current Electronic Fetal Monitoring (EFM) which relies on fetal heart rate – a less predictive measure for fetal complications than direct monitoring of oxygen levels. The device would stretch across the abdomen as pictured and like current pulse oximetry technology use a mix of LEDs and photodiodes (light sensors) to send light to reflect off abdominal and fetal tissue and get a mixed maternal-fetal signal of oxygen saturation. Using signal processing, the fetal signal can be isolated to get a diagnostic metric of fetal oxygen saturation.
Anatomy of Signal Penetration through Tissue
Arrangement of Sensors and LEDs in the Device
Using an optimized placement of LEDs and Photodiode sensors, maternal signals and mixed fetal-maternal signals can be obtained using the device. Two LEDs are used at the signal origin, one emitting near infrared wavelengths (850 nm) and one emitting infrared (740 nm). These are reflected by oxygenated and deoxygenated blood respectively. The intensity of the reflection of each signal is measured by the photodiodes, and the ratio of the oxygenated and deoxygenated components is used to calculate the percentage of oxygen saturation. In the device, we can have a range of photodiode placements. The original design utilizes 5 different photodiodes to be placed near the sensor and around the abdomen to maximize signals obtained and minimize noise. The photodiode close to the LEDs in the center obtain a maternal signals from a shallow reflection through maternal tissue, while far photodiodes get mixed signals.
Performance of Our Signal Processing Algorithms on Hypoxic and Normal Datasets
Diagram of Emitting and Sensing Electronic Circuits
Signal processing utilized recursive least squares (RLS) adaptive noise cancellation to isolate fetal signals which then are passed through a fast fourier transform to extract AC and DC components. These values can then be passed through the below equations to extract oxygen saturation (SpO2). When our signal processing algorithm was testing on a sample dataset of pregnant mothers, they were accurate within 2% for both normal and hypoxic samples. The device was also tested on phantom tissue samples where agarose containing sheep’s blood was placed alternatingly with regular agar to mimic abdominal tissue layers on top of the device, as pictured. The device was found to penetrate 6 cm into the phantom tissue while obtaining consistent, accurate signals.